Autoimmune & Inflammatory Disorders
Autoimmune & Inflammatory Disorders
At Rheumatology Institute, we specialize in diagnosing and managing a wide range of autoimmune and musculoskeletal conditions. Our goal is to relieve symptoms, improve function, and enhance your quality of life through comprehensive, personalized care.

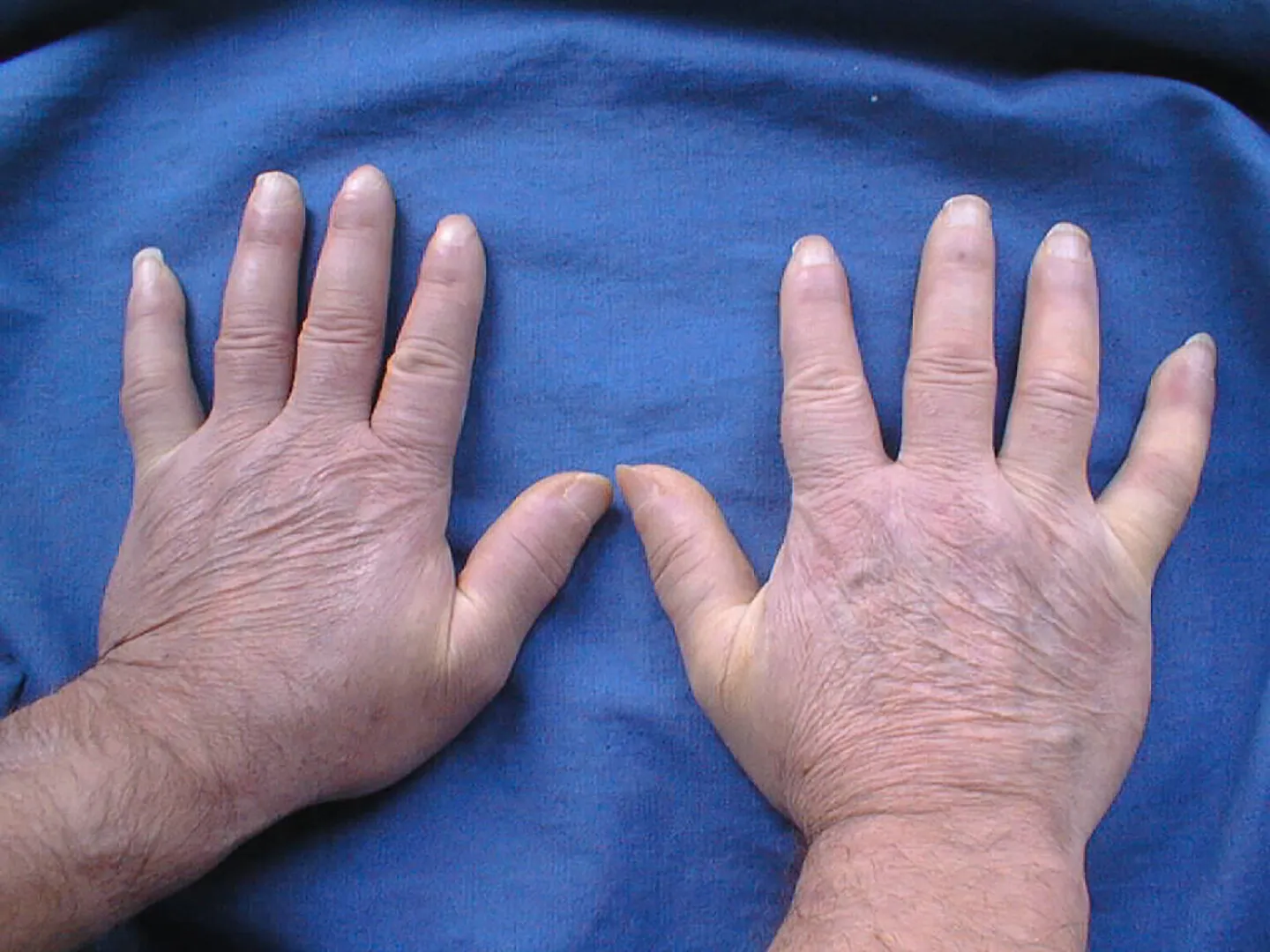
Rheumatoid Arthritis
Rheumatoid Arthritis (RA) is a chronic autoimmune disease that primarily targets the joints, causing persistent inflammation, pain, stiffness, and swelling. Over time, it can lead to joint deformity and loss of function if not properly treated. RA can also affect other systems, including the eyes, lungs, and cardiovascular system. At Rheumatology Institute, we focus on early diagnosis and aggressive treatment using disease-modifying antirheumatic drugs (DMARDs) and biologics. Our goal is to reduce inflammation, prevent joint damage, and improve quality of life. We provide personalized treatment plans and ongoing monitoring to ensure optimal outcomes.

Lupus (Systemic Lupus Erythematosus)
Lupus is a complex autoimmune condition where the immune system mistakenly attacks healthy tissues, affecting skin, joints, kidneys, brain, and other organs. Symptoms can vary widely but often include fatigue, joint pain, rashes, and fever. Flare-ups and periods of remission are common, requiring careful disease management. We provide comprehensive lupus care, including immune-suppressing medications, lifestyle guidance, and organ-specific monitoring. Our team works closely with specialists when needed to provide collaborative care. Early intervention helps reduce complications and improve long-term health outcomes.

Psoriatic Arthritis
Psoriatic Arthritis (PsA) is an inflammatory arthritis linked with psoriasis, a skin condition that causes red, scaly patches. PsA can cause joint pain, swelling, stiffness, and nail changes. It can affect any joint and may lead to joint damage if left untreated. PsA may also involve the spine, causing back pain and reduced mobility. We provide targeted therapies including biologics that address both joint and skin symptoms. Our goal is to reduce inflammation, manage pain, and prevent permanent joint damage while improving overall quality of life.

Ankylosing Spondylitis
Ankylosing Spondylitis (AS) is a type of arthritis that primarily affects the spine, leading to inflammation, chronic back pain, and stiffness. Over time, it can cause the vertebrae to fuse, resulting in reduced mobility and a hunched posture. AS may also affect the eyes and other joints. We offer anti-inflammatory medications, physical therapy referrals, and advanced biologic treatments to help manage symptoms and maintain spinal flexibility. Early treatment is crucial to preserving posture and preventing complications.

Osteoarthritis
Osteoarthritis (OA) is the most common form of arthritis, resulting from the breakdown of joint cartilage and underlying bone, leading to pain, stiffness, and loss of movement. It commonly affects the knees, hips, hands, and spine. OA develops gradually and may worsen with age or overuse. While there is no cure, our treatment focuses on managing symptoms through joint injections, physical therapy referrals, medications, and lifestyle changes. We aim to enhance mobility, reduce pain, and help patients stay active and independent.

Vasculitis
Vasculitis refers to a group of rare autoimmune disorders that cause inflammation of the blood vessels, affecting blood flow and damaging organs. It can impact small, medium, or large vessels and lead to symptoms such as fatigue, fever, weight loss, and organ dysfunction. Types include Giant Cell Arteritis, ANCA-associated vasculitis, and others. Our team uses blood tests, imaging, and biopsies to diagnose the specific type. Treatment often includes corticosteroids and immunosuppressive agents to control inflammation and preserve organ function.

Sjogren’s Syndrome
Sjogren’s Syndrome is an autoimmune disorder that primarily targets the glands that produce moisture, leading to dry eyes and dry mouth. It may occur alone or alongside other autoimmune diseases like lupus or rheumatoid arthritis. Other symptoms can include joint pain, fatigue, and organ involvement. We provide supportive therapies such as artificial tears and saliva stimulants, as well as immunomodulators when systemic symptoms are present. Regular monitoring is key to managing complications like dental decay or lung and kidney issues.
Scleroderma
Scleroderma is a chronic autoimmune disease characterized by hardening and tightening of the skin and connective tissues. It can be localized to the skin or affect internal organs such as the lungs, heart, and digestive system. Symptoms include Raynaud’s phenomenon, skin thickening, and gastrointestinal issues. Our multidisciplinary approach focuses on managing specific organ systems, reducing immune system activity, and improving daily function. Early diagnosis and intervention are vital to limit disease progression and maintain quality of life.

Myositis (Polymyositis and Dermatomyositis)
Myositis is a group of rare autoimmune diseases, including polymyositis and dermatomyositis, that cause inflammation and weakness of the muscles. Dermatomyositis may also present with a distinctive skin rash. These conditions can affect swallowing, breathing, and overall mobility. We use blood tests, imaging, EMG, and muscle biopsies to make a diagnosis. Treatment involves corticosteroids and immunosuppressive drugs to control inflammation and restore muscle strength. Physical therapy plays a vital role in recovery and maintaining muscle function.

Mixed Connective Tissue Disease (MCTD)
MCTD is a rare autoimmune disorder that combines features of lupus, scleroderma, and polymyositis. It commonly causes joint pain, muscle weakness, fatigue, Raynaud’s phenomenon, and hand swelling. The presence of anti-RNP antibodies helps confirm the diagnosis. Symptoms can affect multiple organ systems, including the lungs and heart. Early treatment with immunosuppressants is important to reduce inflammation and prevent complications. Regular follow-up with a rheumatologist helps manage symptoms and maintain function.

Giant Cell Arteritis
Giant Cell Arteritis is an inflammatory condition of the arteries, often affecting the head and neck. It typically occurs in individuals over 50 and presents with headaches, scalp tenderness, jaw pain, and vision changes. Without treatment, it can lead to vision loss or stroke. Diagnosis may involve blood tests, imaging, and artery biopsy. Prompt treatment with corticosteroids is essential to control inflammation and prevent complications. Ongoing monitoring is needed for long-term management.

Granulomatosis with Polyangiitis (GPA)
GPA is a rare autoimmune disease that inflames small- to medium-sized blood vessels, affecting the sinuses, lungs, and kidneys. Symptoms may include sinus pain, chronic cough, fatigue, and joint discomfort. Blood tests often show ANCA antibodies, aiding diagnosis. Without treatment, it can cause serious organ damage. Immunosuppressive medications are used to manage inflammation and control disease activity. Regular rheumatologic care is vital for monitoring and long-term disease control.
